
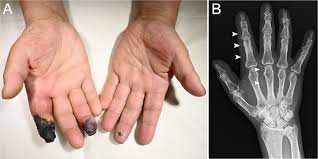

Acral Dry Gangrene is a form of tissue death (gangrene) that typically affects the extremities—especially fingers, toes, ears, or the tip of the nose. It is characterized by dry, blackened, and shriveled skin in the affected area. Unlike wet gangrene, dry gangrene is not associated with infection but results from severe and prolonged lack of blood supply.
🔍 Causes of Acral Dry Gangrene
The primary cause is ischemia (lack of blood flow), often due to:
Peripheral arterial disease (PAD) – especially in diabetic or elderly patients.
Atherosclerosis – narrowing of arteries due to plaque buildup.
Frostbite – prolonged exposure to freezing temperatures.
Embolism or thrombosis – sudden blockage of blood vessels.
Vasculitis – inflammation of blood vessels.
Autoimmune diseases – e.g., Systemic sclerosis (Scleroderma).
Ergot poisoning or long-term ergotamine use (vasoconstriction).
Use of vasopressor medications (e.g., in ICU settings).
Buerger’s disease – common in young male smokers.
🔬 Pathophysiology
Blood supply is cut off to a localized area → tissues receive no oxygen/nutrients → cells die.
The area becomes dry, cold, and discolored due to necrosis.
Because there’s no bacterial infection, there’s no pus or swelling.
Over time, a clear line of demarcation forms between dead and healthy tissue.
🧪 Clinical Features
Cold, dry, and shrunken skin.
Dark brown to black discoloration.
Mummified appearance.
Clearly demarcated from healthy skin.
No significant odor (unlike wet gangrene).
No systemic signs of infection (e.g., fever).
⚕️ Diagnosis
Clinical examination – primary method.
Doppler ultrasound – to assess blood flow.
Angiography – to identify vascular blockages.
Blood tests – to rule out infection or underlying systemic disease.
🩺 Management
Treat underlying cause – e.g., control diabetes, stop smoking, treat vasculitis.
Improve circulation (if possible) – medications or revascularization.
Amputation – often necessary to remove necrotic tissue.
Supportive care – pain management, wound care.
Avoid antibiotics unless secondary infection is suspected.
🚨 Complications
Spread of necrosis to adjacent tissue.
Delayed wound healing.
Need for higher-level amputation.
Functional disability or disfigurement.
📝 Differential Diagnosis
Wet gangrene (infected and foul-smelling)
Necrotizing fasciitis
Frostbite
Severe Raynaud’s phenomenon
